The hip joint is one of the largest joints in our body and is a common area that people can experience pain. There are many reasons as to why hip pain occurs, including osteoarthritis and referral from other areas of our body such as the lower back and the sacroiliac joint. A physiotherapist assessment can assist diagnosis and planning for appropriate injury management and rehabilitation.
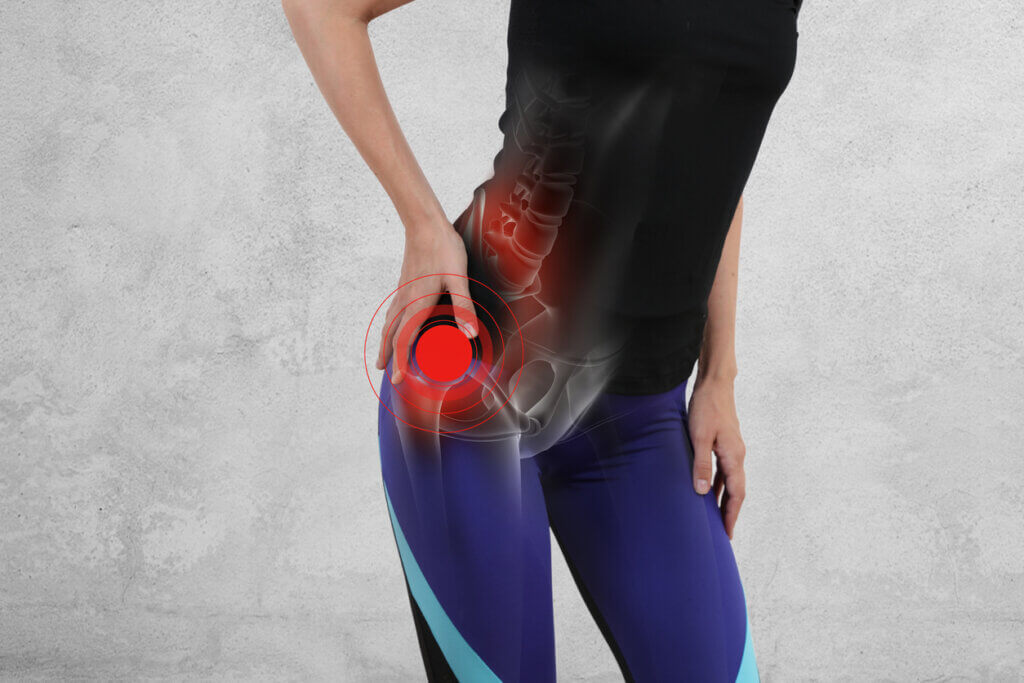
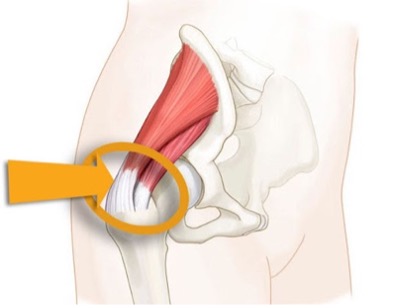
This blog will focus on pain experienced over the lateral hip; this is also commonly referred to as a gluteal tendinopathy. This condition was previously known as hip or trochanteric bursitis. It was thought that the bursa (small fluid filled sac over the outer prominent hip bone that help to cushion and reduce friction in the area) was inflamed.
Recent advances in research and MRI scans have found that this can still occur, although it is a secondary development in response to a gluteal tendinopathy.
The gluteal muscles (gluteus medius and minimus) run from the pelvis and attach onto the outer prominent hip bone. These two muscles primarily act to abduct your hip in a non-weight bearing position, or, more importantly, stabilize the pelvis in a weight bearing position. This can include performing our daily tasks such as walking, running, changing direction on one leg, standing or hanging on your hip, and performing steps/stairs.
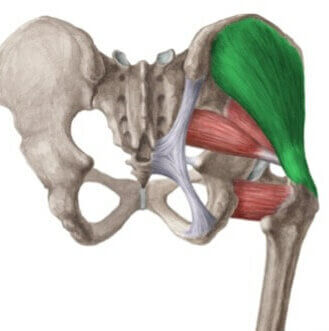
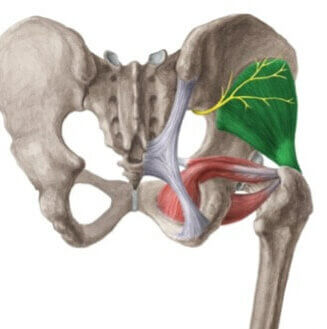
When the gluteal tendons are overused, or asked to do more than they can tolerate, this can lead to a tendinopathy. Tendinopathy is the term used to describe when the tendon fibres become disorganised, which leads to pain and weakness.
Gluteal tendinopathy is more common in women, especially those aged between 40-60 years. Women in this age bracket are three times more likely than men to experience this injury. This can be due to several factors, including women naturally having a wider pelvis than men and women experiencing hormonal changes that occur during the peri menopause and menopause life stages. Other significant risk factors for developing this injury include a change in a person’s standing, walking, or running loads.
Common symptoms of gluteal tendinopathy include pain over the lateral or outer aspect of the hip. This can be worsened with prolonged standing, prolonged walking and walking up inclines, sitting in low chairs, performing repeated steps/stairs and when sitting with the legs crossed for extended periods. It is also common to experience night pain when lying on the affected side. This does not mean these tasks are inherently bad for the hip and should be avoided. Rather, it highlights the importance of pacing – this means limiting big spikes in these types of activities so that the tendon can manage.
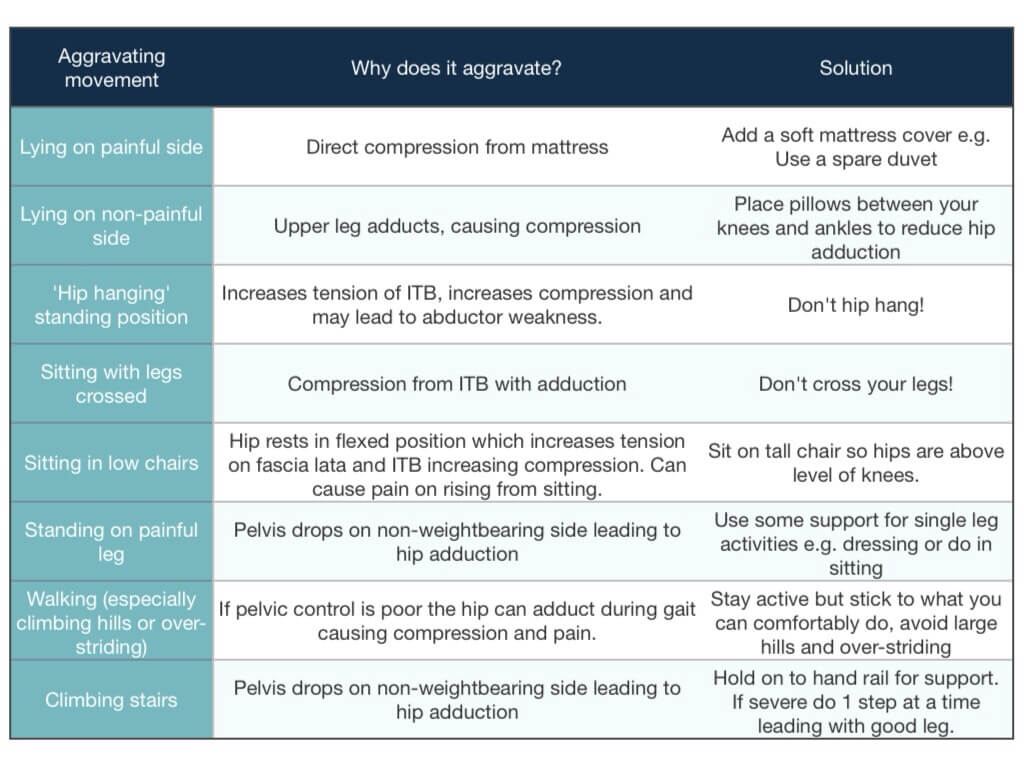
Below is a table that shows activities that can be modified to reduce load on the gluteal tendons.
Physiotherapy has been found to be very effective in the management of gluteal tendinopathy. After a thorough assessment, a physiotherapist will help identify any overload issues that may have contributed to this injury and educate you on how to best manage these aggravating factors. Reducing the amount of load experienced by the gluteal tendons this will reduce irritation and settle symptoms.
In some cases, patients may be recommended a cortisone injection, this may help to reduce pain which can provide a window of opportunity to enable a thorough strengthening program to be completed. Although this intervention is not always effective or appropriate for every individual.
A key component to successful rehabilitation of a gluteal tendinopathy is building the capacity of the tendons to better tolerate loading based activities. This is achieved by commencing a progressive strengthening program of the gluteal and other lower limb muscles. These exercises should be appropriately challenging and pain tolerable. This process can take 3 months if the individual is dedicated to a consistent exercise regimen.


